Retinal organoids, an essential cell bank in the fight against rare retinal diseases
For the International Rare Disease Day, Olivier Goureau, Director of Research in Retinal Development and Regeneration, answers 5 questions about these biological tools that have led to major advances in biology and medicine.
What is the definition of an organoid?
It's a 3D structure, grown in vitro, which reproduces the architecture of an organ and, if possible, some of its functions, using human cells. The name "mini-organ" is often used, but I prefer to talk about an avatar of an organ, an avatar of the retina. The term 'mini-organ' might suggest that we could replace our organs with complete transplants, but this is not the case.
Why is this technology essential for research into rare diseases?
The development of new therapies requires the use of an animal model which recapitulates the clinical signs seen in humans. In the case of rare retinal diseases, we very rarely have animal models. The organoid therefore offers the only alternative capable of providing knowledge of the disease and proof of concept (proof of efficacy) of a therapy. As it is created from a patient's cells, it will carry the mutation and the same clinical signs or phenotypes as the patient. We will therefore be able to specifically study and model a rare disease, with its mutations, and test possible therapies. We save a lot of time.
Research into rare diseases is one of the spearheads of the Institut de la Vision. How does this ecosystem benefit your work?
The advantage of the Institut de la Vision is that we work in collaboration with several teams, such as :
- Isabelle Audo and Christina Zeitz, who are studying large cohorts of patients to identify the genetic anomalies that cause hereditary retinal diseases. We therefore have access to patient cells carrying different mutations. We can build up a database ;
- Kate Grieve, who has created an imaging module that enables retinal organoids to be studied in real time: to observe the mechanisms of a disease, its progression and the degeneration it induces, at the level of the cell, and to assess the impact of a therapy by monitoring the organoid treated.
How is an organoid made?
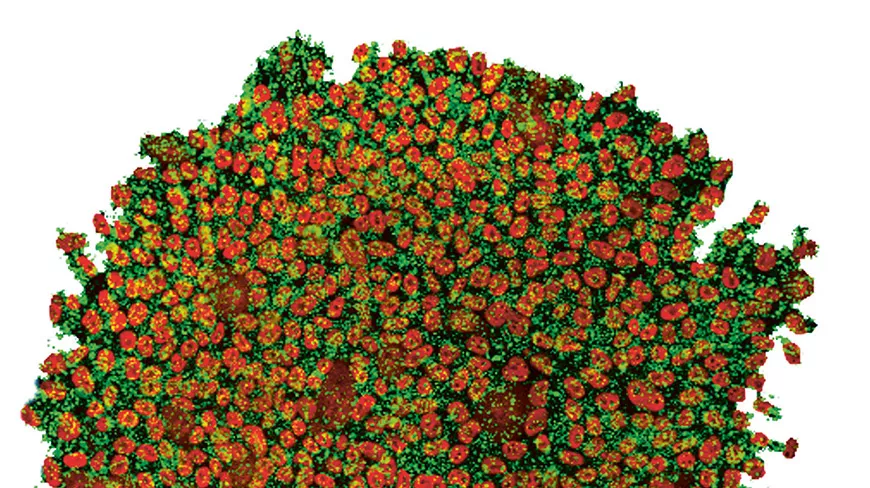
Initially, the organoid can be produced solely from stem cells, which are capable of multiplying and organising themselves. These cells exist in certain human tissues, but not in the retina. At the Institut de la Vision, my team and I have patented a technique for transforming pluripotent* stem cells present in the skin into a retinal organoid that contains all the cell types of the retina (photoreceptors: cones and rods; ganglion cells, glial cells, pigment epithelium cells, etc.). We have trained a number of researchers in our technique and it is benefiting other centres around the world.
Can an organoid help to repair the retina?
As well as being a fantastic living material for deciphering diseases, organoids open up encouraging prospects in the field of :
Cell therapy: the aim is to use the organoids as a source of healthy photoreceptors (not carrying a mutation) and then transplant them into the patient's retina. This approach to replacing cells affected by the disease is currently being studied, but there is still a long way to go. The challenge of our research is to find out whether the restoration of vision will be sufficient and satisfactory.
Gene therapy: we have recently shown that we can prevent the death of photoreceptors in cases of retinopathy pigmentosa. The gene-drug was introduced into the diseased organoid using a viral vector. This is a major breakthrough and an excellent proof of concept that opens up the prospect of clinical trials and the development of a treatment.
*Pluripotent stem cells: cells that have the capacity to give rise to all cell types.
