Discovery of the IDH3G Gene: New Hope for Patients with X-Linked retinitis pigmentosa
At the Institut de la Vision in Paris, the team led by Isabelle Audo and Christina Zeitz has identified a new gene involved in a rare form of X-linked retinitis pigmentosa (RP). This groundbreaking discovery, published in Genetics in Medicine, paves the way for improved diagnosis and the development of targeted treatments.
Retinitis Pigmentosa: A Genetic Disease with Severe Consequences
Retinitis pigmentosa (RP) is a rare inherited disease that affects approximately 1 in 4,000 people. It causes a progressive degeneration of photoreceptors (the light-sensitive cells in the retina), leading to night blindness, followed by a gradual loss of peripheral vision, and ultimately complete blindness.
X-linked forms primarily affect men and account for about 15% of RP cases.
So far, only three genes—RPGR, RP2, and OFD1—have been identified as causes of X-linked RP. However, numerous unexplained cases suggested the involvement of additional genes.
A Major Scientific Breakthrough: The key role of IDH3G
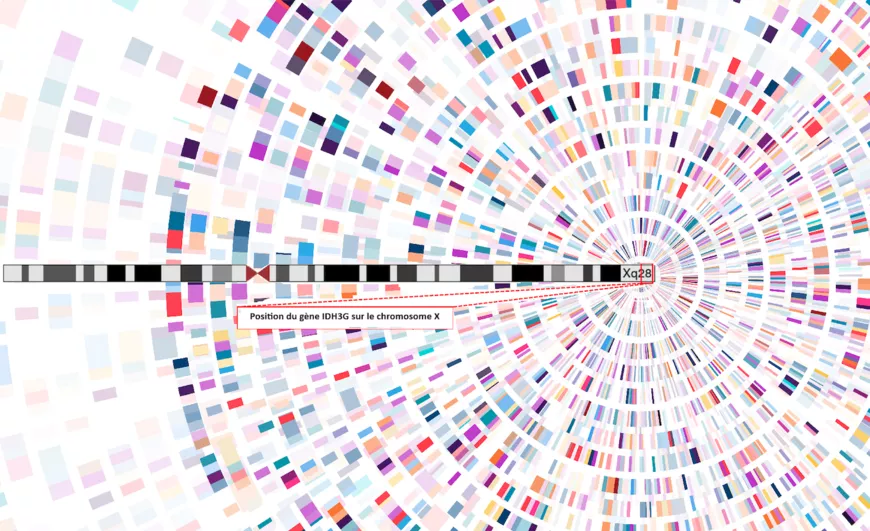
In this study, researchers identified mutations in the IDH3G gene, located on the X chromosome, in five patients with X-linked RP, including some from the large cohort at the National reference center for rare eye Diseases (Hôpital National des 15-20, Paris).
This gene encodes a subunit of isocitrate dehydrogenase 3 (IDH3), an enzyme crucial for energy production in retinal photoreceptors. This enzyme functions in the mitochondria, the cell's energy powerhouse. When IDH3G is mutated, the enzyme malfunctions, leading to energy deficits in photoreceptors and, over time, their degeneration.
"This study highlights the crucial role of mitochondrial metabolism in retinal degeneration. Other IDH3 mutations have been associated with RP, and our findings reveal the involvement of a new key subunit essential for photoreceptor function. Surprisingly, these mutations cause isolated RP without affecting other tissues, despite the gene being expressed elsewhere. This could depend on the mutation type (hypermorphic or not) and underscores the metabolic demand essential for photoreceptor homeostasis. Further studies are needed to explore these hypotheses."
— Christina Zeitz
"The involvement of this protein, which is essential for photoreceptor survival, could open up new therapeutic possibilities targeting mitochondrial function."
— Isabelle Audo
A crucial advance for patients
Currently, treatment options for RP remain very limited. The identification of IDH3G as a causative gene provides new hope for improving genetic diagnosis of unexplained RP cases and developing novel therapeutic strategies, including gene therapies aimed at compensating for or correcting IDH3G dysfunction.
This discovery offers promising therapeutic perspectives, leveraging strategies already explored for other RP forms. Some approaches aim to correct the genetic defect, while others target common degeneration mechanisms independent of the genetic cause. Specifically, targeting mitochondrial metabolism—via IDH3G—could represent a new avenue to slow retinal degeneration.
This breakthrough is part of a series of major recent discoveries: less than a year ago, the same team led by Isabelle Audo and Christina Zeitz identified UBAP1L, a gene whose mutations contribute to certain genetic retinal dystrophies. Thanks to their work, research continues to progress, deepening our understanding of retinal degeneration mechanisms and paving the way for future treatments.
📄 Lorenzo Bianco et al., "Identification of IDH3G, encoding the gamma subunit of mitochondrial isocitrate dehydrogenase, as a novel candidate gene for X-linked retinitis pigmentosa" - Genetics in Medicine, 2025
🔗 Link: https://www.sciencedirect.com/science/article/pii/S1098360025000656?via%3Dihub
About the Study
This research was conducted by a team from the Institut de la Vision (Sorbonne University, Inserm, CNRS) and Hôpital National des 15-20 in collaboration with the Institute of Neurosciences (Montpellier), the University Hospitals of Montpellier and Lille, and international institutions including the San Raffaele Institute (Milan), the Ocular Genomics Institute (Harvard Medical School, Boston), the Arab University of Beirut, and the University of Pittsburgh, under the direction of Isabelle Audo and Christina Zeitz.
