Fighting eye pain, a unique research project in France
"We are working to identify the anatomical pathways involved in chronic eye pain, as well as neuroinflammatory mechanisms, with the goal of discovering new therapeutic targets to provide relief to patients." Annabelle Réaux-Le Goazigo, Inserm Research Fellow at the Institut de la Vision.

Eye pain, a little-known disease
Eye pain is one of the most common causes of ophthalmology consultations. This is not surprising because the cornea is the most densely innervated tissue in the human body. It is estimated that 7,000/mm2 of corneal nerve endings are dense in humans. By comparison, this nerve density is 30 times greater than that of the dental pulp and 500 times greater than that of the skin. It is thus understood that any alteration, stimulation or abrasion of the cornea can lead to severe pain. Dry eye is the most common cause of pain, affecting 20 to 30% of the population over the age of 50 permanently or intermittently. This pathology of the anterior segment of the eye is characterized by pain sensations varying in intensity, ranging from simple discomfort to pronounced eye pain.
Eye pain can be of a nature of:
- inflammatory, usually triggered by tissue damage, leading to an activation of immune cells releasing pro-inflammatory and pro-algic substances which will then stimulate the corneal nerve endings generating a pain message (nociceptive).
- neuropathic, caused by damage or dysfunction of the corneal nerves that become hyperactivated, continuously transmitting nociceptive signals to the brain. Complex in diagnosis, its treatment often requires a multidisciplinary approach, even though there are, to date, no therapeutic recommendations for corneal neuropathic pain.
The pathophysiological mechanisms of eye pain, of nervous and/or inflammatory origin, remain little known today. This observation requires a deepening of our fundamental and clinical knowledge on the anatomy of the corneal nociceptive system (network of nerve endings of the nervous system that gives the alarm and transmits pain to the brain via an electrical signal) and on the cellular mechanisms involved in the initiation and chronicization of ocular pain.
The Institut de la Vision, spearheading research on eye pain
The Institut de la Vision has the only team in France and one of the few in the world to study eye pain. Annabelle Réaux-Le Goazigo and her team aim to identify the cellular and molecular mechanisms involved in the initiation and chronicization of ocular pain, in order to improve current therapies and discover new therapeutic avenues that are sorely lacking.
Many challenges have already been overcome:
- How to assess corneal nerve dysfunctions? Our team has accomplished a unique feat by recording the electrical activity of these nerves in mice, a world first. These recordings not only revealed functional abnormalities such as hyperexcitability and hyperactivation, but they were also critical in evaluating the effectiveness of new treatments to relieve pain.
- What are the mechanisms that lead to the chronicization of pain?
Major advances have also been made in understanding the cellular and molecular mechanisms underlying persistent eye pain, as well as in identifying and validating promising therapeutic targets, offering real hope for patients.
The research has made it possible not only to identify corneal neurons using 3D imaging, developed at the Institut de la Vision, but above all to characterize the cellular and molecular changes occurring in these neurons under pathological conditions.
In addition, recent work has shown that chronic eye pain leads to brain cell changes. These alterations result in an activation and spatial reorganization of microglial cells (inflammatory cells – in red) near neurons (in green) activated during eye pain.
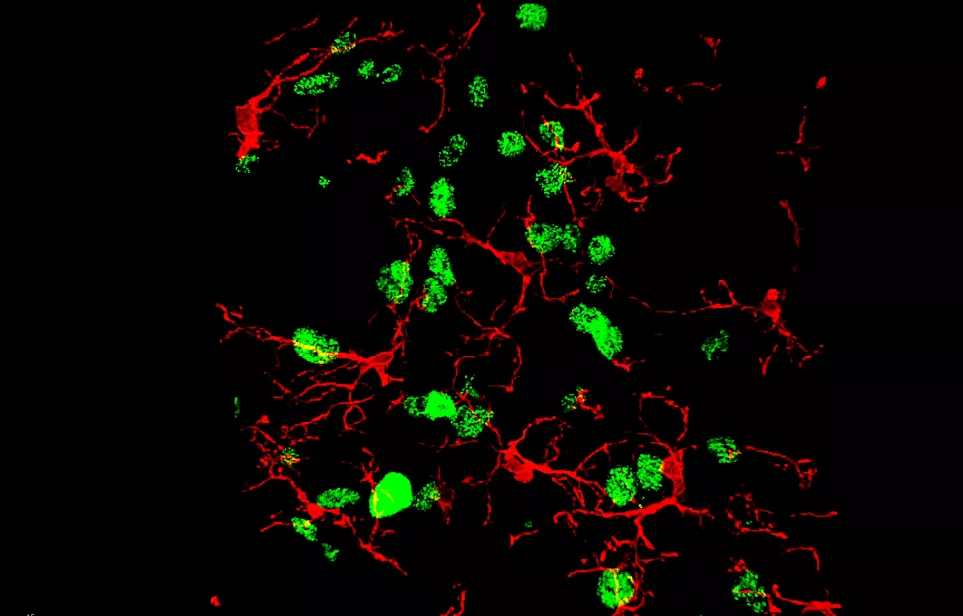
Microglial cells (inflammatory cells, in red) near neurons (in green) activated during eye pain.
At the same time, molecular biology analyses reveal an increase in the expression of many pro-inflammatory genes in the brainstem, a structure involved in the transmission of painful information. These explorations are actively continuing in order to better understand these central mechanisms, which may contribute to the chronicization of eye pain.
Ultimately, these studies aim to precisely identify the neural networks involved in chronic eye pain, thus paving the way for selective and specific therapeutic strategies to inhibit the transmission of painful information..
Translational research, to identify biomarkers
Annabelle Réaux- Le Goazigo's team works in close collaboration with the clinician-researchers of the Clinical Investigation Center dedicated to ocular surface pathologies directed by Prof. Christophe Baudouin and the medical biology and ophthalmo-biology laboratory of the National Hospital of 15-20 (directed by Dr. Françoise Brignole-Baudouin). The center studies a large cohort of patients who participate in clinical studies on vision pathologies.
This collaboration makes it possible, through a multimodal approach, to perform an extremely accurate clinical assessment of the ocular surface in patients suffering from chronic pain associated with dry eye. These data will provide a unique opportunity to identify possible biomarkers of eye pain, paving the way for more targeted diagnostic and treatment strategies.
In the long term, ongoing translational research will deepen our knowledge of this highly disabling pathology and open up new perspectives for the discovery of innovative therapeutic targets, aimed at effectively relieving patients.
For patient information: if you suffer from chronic eye pain, the National Hospital of 15-20 welcomes you by appointment and with referral from your ophthalmologist. Contact: douleur@15-20.fr

Dr Annabelle Réaux-Le Goazigo, Inserm Researcher at the Institut de la Vision, is a neurobiologist with internationally recognized expertise in the field of pain.
Her basic and clinical research projects, carried out in collaboration with the Clinical Investigation Center of the National Hospital of 15-20, aim to deepen our knowledge of the peripheral and central mechanisms associated with chronic eye pain.
